Well, over the last few weeks, I've been struggling at various fronts about the laws slowly being implemented which would make it quite difficulty for healthcare institutions and providers to be in the service of improving health in the country especially for the common man.
It is of course true that we boast world class facilities in healthcare such that 'Medical Tourism' has become a very common term for many a corporate hospitals. But, the fact remains that the doctor : population ratio remains abysmally low in almost a majority part of the country. More so, as I mentioned in a previous post, the consultant : population is all the more in a precarious state.
Over the last couple of years, I've been trying to push the need for Family Medicine consultants as well as Maternal & Child Health consultants in the country on a larger scale to cater to primary and secondary health care needs of the population. Although the National Board of Examinations have accredited DipNB in Family Medicine and Maternal & Child Health, there has not been much of an encouraging response from the Medical Council of India.
In fact, it is not very difficult to come to a conclusion that healthcare in India would benefit much from the presence of more Family Medicine and Maternal & Child Health consultants rather than other speciality consultants.
Just one incident and a thought which went through me when it comes to issue of consultants managing all cases pertaining to a specific speciality. Now, as I had mentioned about this in a previous post, I put my arguments in the light of the high densely populated regions of rural India where even the presence of a doctor with an MBBS degree is a luxury.
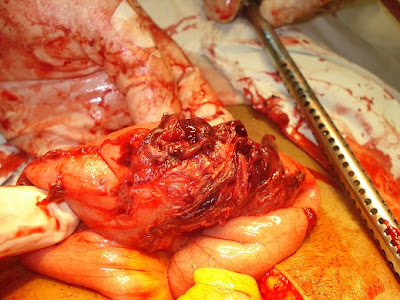
Yesterday, I had a call from our Insurance Provider of RSBY. He wanted reason why we did a Osteotomy Femur of a young man who had been struggling with the condition for almost 5 years. This guy had a accessory piece of bone jutting out from the lower aspect of his thigh. He had multiple episodes of injury. The treatment was to remove it. The problem was that he had gone to couple of orthopedicians and all of them wanted a hefty amount which his family was unable to afford.
Then, he came to find out about NJH being empanelled under RSBY. He wanted to know if this surgery could be done. Our surgeon, Dr Nandamani was confident that he could do it. The young man underwent the procedure and is doing fine. Now, our Insurance Provider wants to know why we did the surgery without an orthopedician.
I asked the local fellow on whether he had an orthopedician empanelled under the scheme in the nearby region. The answer was no. The complete truth was that there was an orthopedician who was empanelled under the scheme last year, but he had come to the conclusion that RSBY was not paying him enough and decided not to continue it when the option for re-empanelling arose.
The other option would be to go to Ranchi and find out an RSBY empanelled orthopedician and get the surgery done. But, that involves quite a lot of overhead expenses which the insurer would not pay. Therefore, he got the surgery done at NJH.
Now, I thought of doing the same exercise I did for the obstetricians in the last post. The question was about the ideal orthopedician : population ratio. Well, as per my information, there are 3 orthopedicians in the whole of Palamu, Latehar and Daltonganj.
Now, coming to the thought that crossed my mind last week
I hope all of you know about the Medical Termination of Pregnancy Act of the Government of India. I remembered the clauses which stipulate on who can do an abortion. I could not believe when I contemplated on the same. In addition to an obstetrician, any doctor who has done 6 months of internship in Obstetrics and Gynecology in a teaching institute OR one year of work in Obstetrics and Gynecology department of a hospital OR assisted 25 cases of MTP in an institution recognised for the purpose.
I had studied this many a time for my graduate and post-graduate examinations. But, did you notice the last part. Just assisting 25 cases of MTP would actually give you the 'licence to kill'. And mind you, you could end up killing both, as a MTP is not without any associated danger to the mother.
In the light of this, could we look at procedures which heal. Medical graduates without post-graduate training has been doing yeoman service in many areas of the country in rural areas doing procedures which would cause frantic scenes in the Emergency Rooms of many a super-speciality hospital. In fact, there was one generation of doctors who believed in training up willing medical graduates in all aspects of medical specialities as people in rural hinterlands of the country could never think about going to a superspecility centre.
Unfortunately, very few of our policy-makers are aware about ground realities. They bring in
acts like the CEA where you need consultants of different specialities to attend to a simple physiological condition like a normal delivery.
If the legislature can give the license of kill once a medical graduate observes 25 MTPs, I'm certain that it would be unethical not to give the license to practice any speciality of medicine to a doctor who passes out with a MBBS degree. But, of course - the patient should be well aware of who he is going to. In places like ours which are umpteen in 3rd world countries, a couple of well qualified and experienced medical graduates would be more worth than the hoard of quacks who populate the area.
A common refrain that we here at many of the mission hospitals including NJH. . .
Doctor saab, humlog yeham thak bahut ummid ke sath aye hain . . .Hamare liye ye bahut bada baat hai. Hum aage nahim leke ja sakte. . . Jo karna hai, aapko hi karna hai . . . (Dear doctor, we have come till here with great faith in you. Coming till here is a big achievement for us. We can't go further. Whatever needs to be done, has to be done by you.)
The last one to give me this dialogue was the parent of a little boy for whom we could not come to a diagnosis. Most probably, he had a brain stem tumour. I asked the parents to take him home. He was referred by someone we knew - he died at home 2 days later. . .
So food for thought for the weekend . . . If we can obtain the license to kill our unborn without much difficult, why all the fuss being made about need for specialists especially when you have so few of them . . . more so, when it comes to under-served and remote areas of the country. . .